But why does it happen. Why do some men develop gynecomastia while others never do. The answer is simple in biology and complex in circumstance. Gynecomastia results from an imbalance between testosterone and estrogen. Men produce both hormones. The ratio matters. When estrogen rises or testosterone falls, even slightly, the breast gland can begin to grow. The testosterone ratio and androgen ratio are both important in determining whether gynecomastia develops, as shifts in these ratios can promote breast tissue growth. The adrenal glands also play a role by producing hormones that can be converted to estrogens, contributing to the hormonal imbalance that produces gynecomastia.
Your previous Regeneris writing emphasizes that men deserve a thoughtful explanation and a private plan, not judgment. That is the foundation of this article. Understanding the cause helps remove shame.
There are several categories of causes. Each one tells a different story.
Puberty
This is the most common cause. Teenage boys experience dramatic hormonal swings. Testosterone surges, but so does estrogen. For some boys, the temporary imbalance causes breast tissue to grow. Sometimes it is tender. Sometimes not. In many cases, this resolves within months. But in a significant number of young men, the gland remains permanently. They enter adulthood with a chest shape they have no control over. They assume it is fat. They hide it. They reshape their wardrobes. Gynecomastia from puberty is one of the most common
patterns we see. Early puberty can also trigger transient gynecomastia due to rapid hormonal changes, while prepubertal gynecomastia is rare and requires careful evaluation for underlying
causes.
Aging and Testosterone Decline
As men grow older, testosterone levels decrease gradually. Estrogen does not fall at the same rate. The ratio shifts. This is why older men often develop new breast tissue even when their weight has not changed. The gland grows slowly, sometimes over years, sometimes over months. TRT conversations often intersect with gynecomastia questions because both involve hormone balance. Your prior writing on men’s health describes how testosterone regulates drive, mood, and body composition. That same regulation influences the male chest. When testosterone lowers, estrogen can have more effect.
Medications
Many medications can cause gynecomastia. Some affect hormone production. Others affect hormone metabolism. Others influence receptors. Common culprits include:
- Antiandrogens
- Antidepressants
- Heart medications
- Some antibiotics
- Anti anxiety drugs
- Medications for ulcers or reflux
- Steroids and steroid precursors
Marijuana and alcohol can also influence estrogen metabolism. Men who use anabolic steroids often encounter gynecomastia when they stop. Their natural testosterone shuts down for a time, while estrogen remains active. The tissue grows in that short window and rarely retreats. Drug-induced gynecomastia is a well-recognized phenomenon, as certain medications and substances can produce gynecomastia by altering hormone levels or receptor activity.
This is not a judgment. It is biology responding to chemical signals.
Weight Changes
Obesity does not cause glandular gynecomastia directly, but it influences the hormonal environment. Fat tissue produces aromatase, an enzyme that converts testosterone into estrogen. More fat means more estrogen conversion.
Increased aromatase expression in adipose tissue further elevates estrogen levels, increasing the risk of gynecomastia. Once the gland grows, losing weight will not reverse it. Weight loss helps shape the chest, but it cannot undo gland formation.
Medical Conditions
Some conditions affect the liver, thyroid, or testes in ways that disturb hormone balance. Liver disease can reduce the clearance of estrogen. Thyroid disorders can influence hormone receptors. Testicular tumors can change androgen production. Leydig cell tumors and sertoli cell tumors are rare testicular neoplasms that can secrete hormones and cause gynecomastia. Chronic kidney disease and renal failure can disrupt hormone metabolism, leading to increased estrogen and decreased testosterone, which contribute to gynecomastia. These causes are less common, but they exist, which is why physicians evaluate gynecomastia carefully.
Most men, however, fall into the first three categories. Puberty. Aging. Medications. These explain the overwhelming majority of cases.
A man may ask, “Why me.” It is a fair question. Sometimes the answer is genetic. Some men are more sensitive to estrogen than others. Some have receptors that respond more strongly to small changes. Hormone balance is personal. Two men with the same testosterone levels may experience completely different physical results. This does not reflect weakness. It reflects individuality. When no clear cause is found after thorough evaluation, the condition is termed idiopathic gynecomastia.
Gynecomastia is not a sign of low testosterone alone. Men with normal levels can develop it. It is the local tissue response that matters. Glandular breast tissue has estrogen receptors and androgen receptors. When stimulated, the gland grows. Testosterone does not stop this once it begins. Androgen resistance, where the body’s tissues are less responsive to androgens, can also contribute to gynecomastia even when testosterone is present. A man cannot out train it. He cannot out discipline it.
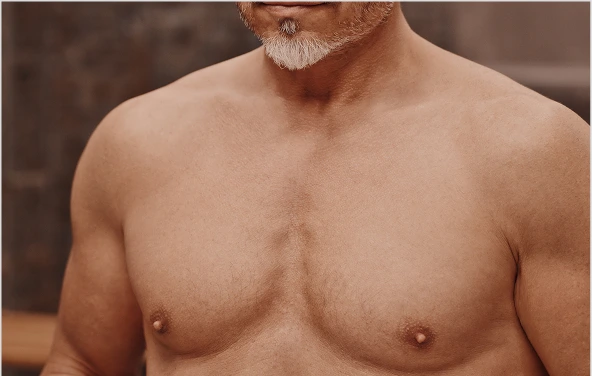
This is why so many men try for years to fix the problem themselves. They lift weights, lose weight, take supplements, restrict calories, and still see the same roundness under the nipple. Some men say, “I got lean everywhere except here.” Others say, “I feel stronger than ever but this part does not change.” They think they did something wrong. They did not.
Understanding the cause helps men understand the treatment. When the issue is glandular,
only surgery removes the gland. When the issue is fat, weight loss or VASER liposuction may help. Often men have both. Removing the gland and sculpting the surrounding fat creates a natural contour. This is visible in the chest sculpting work you describe elsewhere, where regaining confidence is a central theme.
For some men, psychological effects are as real as the physical ones. Gynecomastia can make a man self conscious. It changes how he dresses, how he swims, how he dates, how he stands. One man said, “I kept my shoulders rounded so my shirt would hang differently.” Another said, “I avoided the gym because I did not want anyone to notice.” These stories are not rare. They are extremely common. Painful gynecomastia, where breast pain or tenderness is present, can further impact quality of life and may influence treatment decisions.
But shame does not belong here. Gynecomastia is tissue responding to hormones. It is a medical condition, not a personal failing. Once a man understands this, his view of himself often softens. Understanding invites action.
The practical question becomes this. What should a man do if he notices enlargement in his chest.
- First, he should examine it. Is the tissue soft or firm. Does it feel like fat or something more structured. Has it grown slowly or suddenly. Does one side appear larger. Does it sit directly under the nipple. These small details carry meaning. A thorough breast examination should also assess for breast pain and nipple discharge, as these symptoms may indicate underlying pathology.
- Second, he should review medications and lifestyle. Has he started or stopped any hormonal substances. Is he using cannabis. Has he changed any prescriptions. Is he drinking more. Has he gained or lost significant weight.
- Third, he should be evaluated. Not because gynecomastia is dangerous, but because clarity is helpful. A brief consultation answers the question quickly. Men often feel relief the moment someone explains the difference between fat and gland. Evaluation may include checking hormone levels such as free testosterone, as well as assessing gonadotropin secretion, which can help identify underlying hormonal imbalances.
- Fourth, he should choose a plan. If it is purely fat, weight loss or targeted sculpting can help. If it is gland, surgery is the definitive answer. When done properly, the procedure is simple, discreet, and effective. Men are often surprised by how small the incision is and how natural the result looks. Gynecomastia treated with surgery or medical therapy is most effective when addressed early; once gynecomastia persists for more than two years (chronic gynecomastia), medical
therapy is less likely to work, and gynecomastia surgery may be indicated. Once gynecomastia becomes chronic, surgical intervention is often the best option.
One man said after his correction, “I wish I had known how easy this would be.” Another said, “I spent ten years trying to hide something that took less than an hour to fix.” These are common feelings. The hardest part is not the treatment. It is the years spent misunderstanding the cause.
Gynecomastia arises from hormonal shifts, medications, genetics, and sometimes age. It cannot be corrected by willpower or sweat. Once the gland grows, it remains until removed. Knowing this gives men back control. They can stop blaming themselves. They can understand the biology. They can pick a meaningful solution. Prevent gynecomastia strategies, such as using medications like tamoxifen or aromatase inhibitors in high-risk groups, may help reduce the risk in certain situations.
The reasons for gynecomastia are many, but the path to clarity is simple. Look honestly. Learn the cause. Choose the right fix. The chest can be restored. Confidence can return. Men do not need to carry this quietly.
Special Situations
Hormonal Mechanisms
Testicular and Endocrine Factors
Breast Development and Gynecomastia
Breast development in males is a nuanced process, shaped by the interplay of hormones, genetics, and sometimes medications. While most men have only a small amount of breast tissue, certain factors can trigger the growth of glandular tissue, leading to the enlargement of one or both breasts—a condition known as gynecomastia.
During puberty, it’s common for boys to experience a temporary increase in breast tissue. This pubertal gynecomastia is driven by natural fluctuations in testosterone and estrogen levels. For most, the change is brief and resolves on its own. But for some, the glandular tissue remains, persisting into adulthood and often causing both physical discomfort and emotional distress.
Gynecomastia isn’t limited to puberty. It can develop at any age, and sometimes the cause is more complex. Genetic conditions like Klinefelter syndrome or androgen insensitivity syndromes can disrupt the normal balance of hormones, making breast tissue more likely to grow. Certain tumors—such as testicular tumors or adrenal tumors—can also alter hormone production, leading to breast enlargement. Even some medications, including anabolic steroids and calcium
channel blockers, are known to cause gynecomastia by affecting hormone levels or the way the body processes hormones.
While gynecomastia itself is benign, it’s important to be aware of the rare but real risk of male breast cancer. Men with gynecomastia should pay attention to changes in their breast tissue, such as lumps, nipple retraction, or unusual discharge. Regular breast examinations and prompt medical attention for any concerning symptoms are essential, as early detection of male breast cancer can make a significant difference in outcomes.
Diagnosis of gynecomastia typically involves a thorough physical exam, a review of medical history, and sometimes laboratory tests to check hormone levels and rule out underlying conditions. This careful approach helps distinguish gynecomastia from other causes of breast enlargement and ensures that any serious issues, like testicular tumors or liver disease, are not overlooked.
Treatment for gynecomastia depends on the underlying cause. If a hormonal imbalance is identified—such as low testosterone levels in primary or secondary hypogonadism—medical treatment like hormone therapy may help restore balance and reduce breast tissue. In cases where medications are the culprit, adjusting or discontinuing the drug can sometimes reverse
the changes. For persistent or bothersome gynecomastia, surgical treatment such as male
breast reduction can remove the excess glandular tissue and restore a natural chest contour.
Prevention is possible in some cases. Avoiding substances known to cause gynecomastia, like anabolic steroids, and managing underlying health conditions can reduce risk. For prostate cancer patients undergoing androgen deprivation therapy, the risk of developing gynecomastia is well recognized. In these situations, prophylactic breast radiotherapy or the use of aromatase inhibitors may be recommended to prevent or treat breast tissue proliferation.
Ultimately, understanding the factors that cause gynecomastia empowers men to seek the right care. Whether the issue is pubertal gynecomastia, a side effect of medication, or a sign of a deeper hormonal imbalance, there are effective ways to treat gynecomastia and restore
confidence. Regular breast examinations and awareness of male breast cancer symptoms are important steps in maintaining health and peace of mind.
Peak Masculinity
Starts Here

By Dr. Ryan Welter
December 16, 2025